Overview –
The American Medical Association (AMA) in conjunction with the Centers for Medicare & Medicaid Services (CMS), have announced changes for office and other outpatient E/M services that will go into effect on Jan. 1, 2021. The changes only pertain to office or other outpatient E/M service codes (99202-99215); all other E/M services will remain unchanged.
- The new E/M guidelines are specific to office and other outpatient CPT®1 codes 99202-99215
- The CPT code 99201 will be deleted
- Providers will now select the appropriate E/M code based on either the level of medical decision making (MDM) or total time
- History and examination will no longer be significant in determining the level of service, only when medically appropriate
- Total time is defined as “total time spent on the day of the encounter”
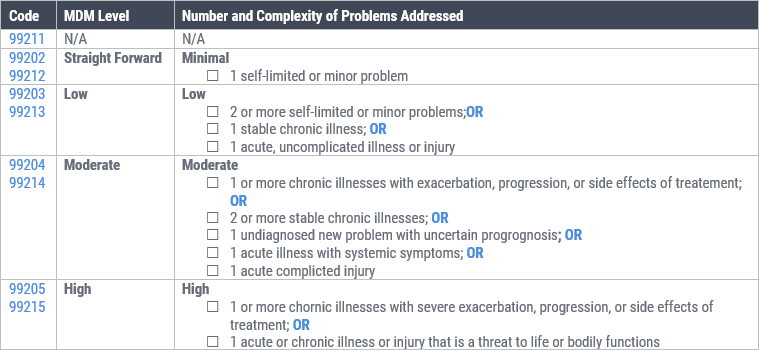
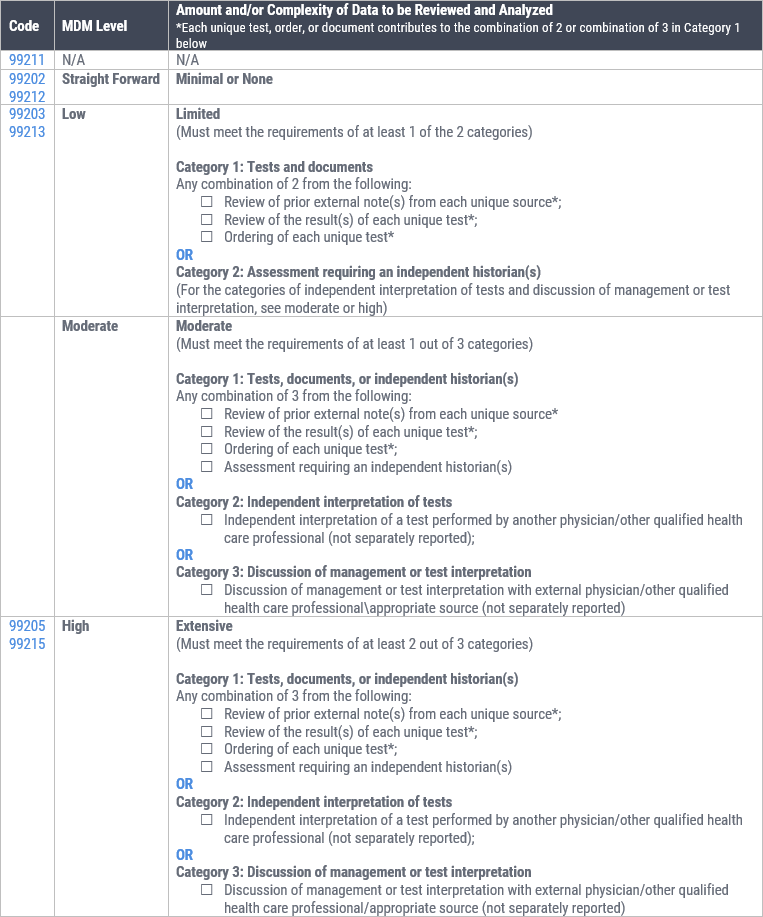
- Revisions to the MDM elements for codes 99202–99215:
- “Number of Diagnoses or Management Options” will change to “Number and Complexity of Problems Addressed”
- “Amount and/or Complexity of Data to be Reviewed” will change to “Amount and/or Complexity of Data to be Reviewed and Analyzed”
- “Risk of Complications and/or Morbidity or Mortality” will change to “Risk of Complications and/or Morbidity or Mortality of Patient Management”
- A new prolonged services code (99xxx) has been created to describe a prolonged office and outpatient E/M service of 15 minutes beyond the total time of the primary E/M code for CPT codes 99205 or 99215.

Selecting an E/M Code Based on Medical Decision Making
Starting on January 1st, 2021, providers may select the level of office and outpatient E/M service based on either Medical Decision Making (MDM) or Time.
Medical decision making is currently part of the Evaluation and Management selection components. However, changes have been made to the elements of medical decision making and the criteria for selection.
Medical decision making includes establishing diagnoses, assessing the status of a condition, and/or selecting a management option. Medical decision making in the office and other outpatient services code set is defined by three elements:
- Problem: The number and complexity of problem(s) that are addressed during the encounter.
- Data: Amount and/or complexity of data to be reviewed and analyzed.
- Risk: Risk of complications and or morbidity or mortality of patient management.
Definitions of MDM Elements
The new guidelines provide updated definitions for the elements of medical decision making for office or other outpatient services.
How To: Select an E/M Code based on the 2021 medical decision making guidelines.
Step 1: Problem
Select the appropriate number and complexity of problems addressed during the encounter.
Step 2: Data
Select the amount and/or complexity of data to be reviewed and analyzed.
Step 3: Risk
Select the risk of complications and/or morbidity or mortality of patient management.

Step 4:
Now put the selections together to determine the appropriate E/M code level as shown in the example below:
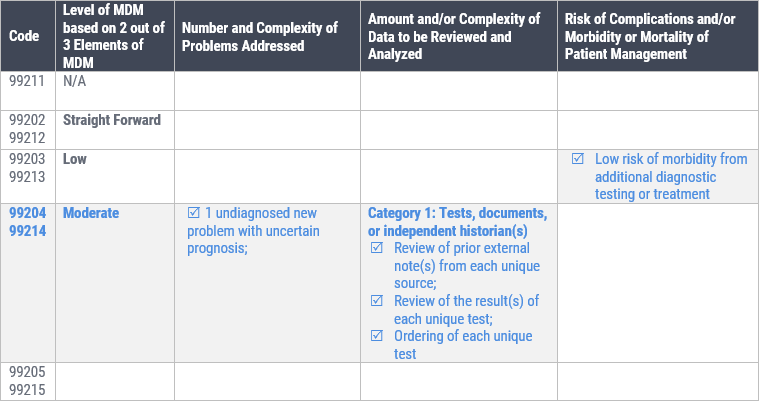
The appropriate code level to select would be level 4 – Moderate (99204 or 99214), as two of the three elements of medical decision making was met within the level category.

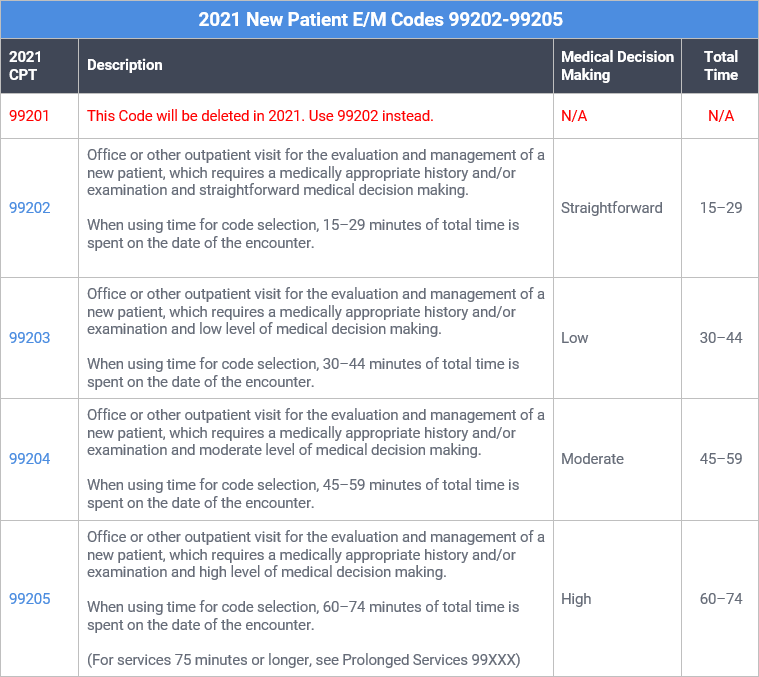
Selecting an E/M Code Based on Total Time
Starting in 2021, for office or other outpatient services (CPT® codes 99202-99205, 99212- 99215), the time for these services is the total time on the date of the encounter. It includes both the face-to-face and non-face-to-face time personally spent by the physician and/or other qualified health care professional(s) on the day of the encounter (includes time in activities that require the physician or other qualified health care professional and does not include time in activities normally performed by clinical staff).
For office or other outpatient services (CPT codes 99202-99205, 99212- 99215), time may be used to select a code level whether or not counseling and/or coordination of care dominates the service. However, time may only be used for selecting the level of the other E/M services when counseling and/or coordination of care dominates the service.
2021 E/M Code Time Intervals
The total time intervals corresponding to New Patient E/M CPT codes 99202-99205 are as follows:
The total time intervals corresponding to Established Patient E/M codes 99211-99215 are as follows:
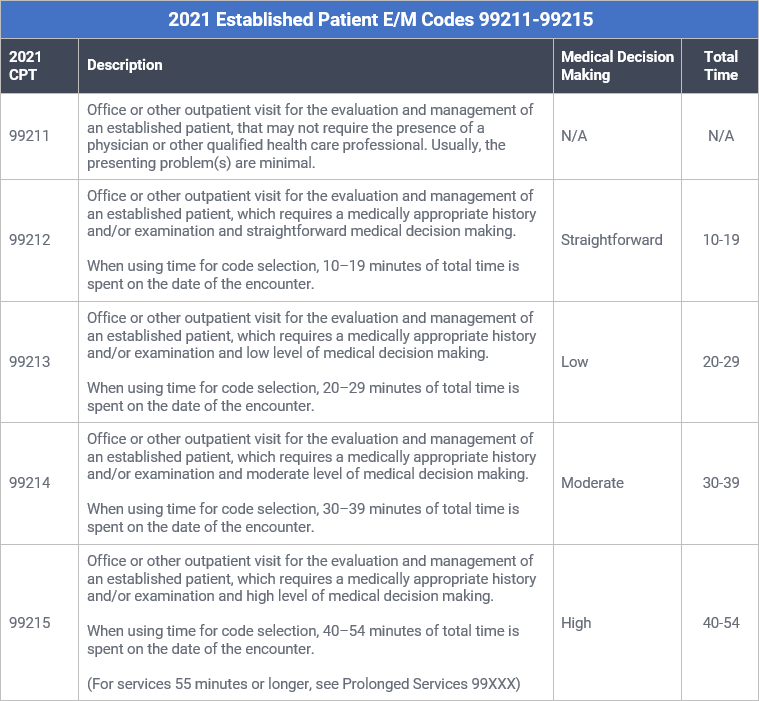
For example, in order to report 99215, 40 to 54 minutes of total time must be spent on the date of the encounter by the physician or qualified health care professional.
Acceptable Time-Based Activities
Physician/other qualified health care professional time includes the following activities, when performed:
- Preparing to see the patient (eg, review of tests)
- Obtaining and/or reviewing separately obtained history
- Performing a medically appropriate examination and/or evaluation
- Counseling and educating the patient/family/caregiver
- Ordering medications, tests, or procedures
- Referring and communicating with other health care professionals (when not separately reported)
- Documenting clinical information in the electronic or other health record
- Independently interpreting results (not separately reported) and communicating results to the patient, family, or caregiver
- Care coordination (not separately reported)
Split and/or Shared Visits
In circumstances where the physician and qualified healthcare professional each perform the face-to-face and non-face to face work for a visit, the time spent by each is summed for the total time.
For example, a physician spends five minutes of time with an established patient and a physician assistant spends 25 minutes on the date of the encounter. The total time of the visit would be 30 minutes (5 + 25); and therefore, CPT code 99214 (30 to 39 minutes) would be selected per the new guidelines.
Prolonged Service With or Without Direct Patient Contact on the
Date of an Office or Other Outpatient Service
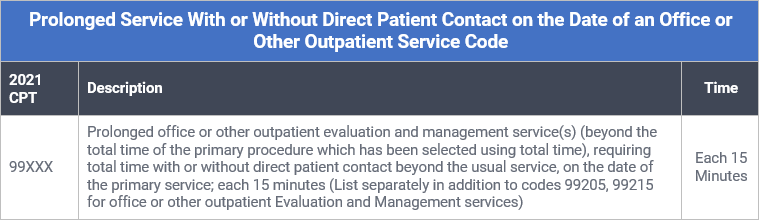
Code 99XXX is used to report prolonged total time (ie, combined time with and without direct patient contact) provided by the physician or other qualified health care professional on the date of office or other outpatient services (ie, 99205, 99215).
Code 99XXX is only used when the office or other outpatient service has been selected using time alone as the basis and only after the total time of the highest-level service (ie, 99205 or 99215) has been exceeded. To report a unit of 99XXX, 15 minutes of additional time must have been attained. Do not report 99XXX for any additional time increment of less than 15 minutes.
Time spent performing separately reported services other than the E/M service is not counted toward the time to report 99205, 99215 and prolonged services time.
Do not report 99XXX in conjunction with 99354, 99355, 99358, 99359, 99415, 99416
Additional Resources
AMA Resources:
Table 2 – CPT E/M Office Revisions Level of Medical Decision Making (MDM)
Revisions to the CPT E/M Office Visits: New Ways to Report Using Medical Decision Making (MDM)
CMS Resources:
1CPT is a registered trademark of the American Medical Association. Copyright 2019 American Medical Association. All rights reserved.
