The Quality Payment Program (QPP) was created by the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. The QPP transforms the Medicare physician payment system from one focused on volume to one focused on value. Clinicians have two tracks to choose from in the Quality Payment Program based on their practice size, specialty, location, or patient population:
MIPS – Merit-Based Incentive Payment System streamlines existing Medicare quality programs including Physician Quality Reporting Program (PQRS), the Value-Based Payment Modifier (VM), and the Medicare EHR Incentive Program (MU) into one program.
APMs –Alternative Payment Model provides alternative pathways for clinicians to participate that incentivizes quality and value.
Under MIPS, clinicians are included if they are an eligible clinician type and meet the low volume threshold (LVT), which is based on allowed charges for covered professional services under the Medicare Physician Fee Schedule (PFS) and the number of Medicare Part B patients who are furnished covered professional services under the Medicare Physician Fee Schedule.
Performance is measured through the data clinicians report in four areas:
- Quality;
- Improvement Activities;
- Promoting Interoperability; and
- Cost
How It Works
Under MIPS, CMS evaluates a clinician’s performance across multiple categories that lead to improved quality and value in our nation’s healthcare system. There are four performance categories that make up your final score. Your final score determines what your payment adjustment will be. These categories are:
Quality
This performance category replaced PQRS. This category covers the quality of the care you deliver, based on performance measures created by CMS, as well as other medical professional and stakeholder groups. You pick the six measures of performance that best fit your practice.
Promoting Interoperability (PI)
CMS has re-named the Advancing Care Information performance category to Promoting Interoperability (PI) to better focus on patient engagement and the electronic exchange of health information using certified electronic health record technology (CEHRT). This performance category replaced the Medicare EHR Incentive Program for EPs, commonly known as Meaningful Use. This is done by proactively sharing information with other clinicians or the patient in a comprehensive manner. This may include: sharing test results, visit summaries, and therapeutic plans with the patient and other facilities to coordinate care.
Improvement Activities
This is a new performance category that includes an inventory of activities that assess how you improve your care processes, enhance patient engagement in care, and increase access to care. The inventory allows you to choose the activities appropriate to your practice from categories such as enhancing care coordination, patient and clinician shared decision-making, and expansion of practice access.
Cost
This performance category replaces the VBM. The cost of the care you provide will be calculated by CMS based on your Medicare claims. MIPS uses cost measures to gauge the total cost of care during the year or during a hospital stay.
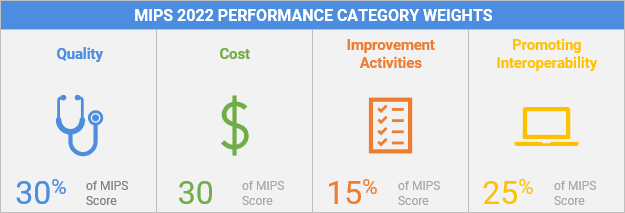
Performance Category Weights
The MIPS performance categories have different “weights” and the scores from each of the categories are added together to give you a MIPS Final Score.
Performance Year
The MIPS performance year begins on January 1 and ends on December 31 each year. If you’re eligible for MIPS, you must report data collected during the calendar year by March 31 of the following calendar year. Payment adjustments, based on the data you submit for services provided, are applied to Part B claims during January 1 to December 31 of the year following data submission. For example, if you collect data between January 1 – December 31, 2022 (the performance year), you must report your data by March 31, 2023, and will receive a MIPS payment adjustment between January 1 – December 31, 2024 (the payment year). Learn more about the MIPS Timeline and Important Deadlines.
For detailed and up-to-date information please visit the Quality Payment Program website.
