Overview
The cost performance category is an important part of MIPS. Although clinicians don’t personally determine the price of individual services provided to Medicare patients, they can affect the amount and types of services provided. By better coordinating care and seeking to improve health outcomes by ensuring their patients receive the right services, clinicians play a meaningful role in delivering high-quality care at a reasonable cost.
CMS uses Medicare claims data to calculate cost measure performance, which means clinicians don’t have to submit any data for this performance category.
There are a total of 25 cost measures available to evaluate the cost category performance in the 2022 MIPS performance year.
- 23 episode-based measures
- Total Per Capita Cost (TPCC) measure
- Medicare Spending Per Beneficiary Clinician (MSPB Clinician) measure
CMS added 5 newly developed episode-based cost measures into the MIPS cost performance category, beginning with the 2022 performance period:
- 2 procedural measures:
- Melanoma Resection
- Colon and Rectal Resection
- 1 acute inpatient medical condition measure:
- Sepsis
- 2 chronic condition measures:
- Diabetes
- Asthma/Chronic Obstructive Pulmonary Disease (COPD)
Each measure is payment-standardized and risk-adjusted. All of the cost measures used the standard CMS-HCC risk adjustment model as a starting point, and the 23 episode-based cost measures include additional measure-specific risk adjustors informed by clinician expert workgroups that provided recommendations during the development of the measures.
In addition, the TPCC measure is also specialty-adjusted.
Each cost measure is attributed to clinicians according to the measure’s unique specifications.
Two measure specifications documents are available for each cost measure:
- A Measure Information Form (MIF) in a PDF file, and
- A measure codes list Excel file.
The MIF describes the methodology used to construct each measure. The measure codes list file contains service codes and clinical logic used in the methodology, including episode triggers, exclusion categories, episode subgroups, assigned items and services, and risk adjustors.
For a further detailed explanation of the Performance Cost Category please refer to the Additional Resources section below.
Reporting/Submission Requirements
CMS will use data from Medicare Parts A and B claims—with dates of service from January 1, 2022 to December 31, 2022—to calculate your cost performance category score.
You do not need to submit any data or take any separate actions for this performance category.
Scoring
Overview
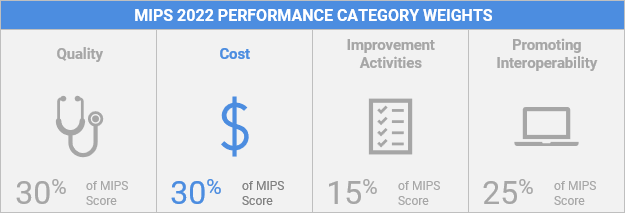
The cost performance category is weighted at 30% for individuals, groups, and virtual groups reporting traditional MIPS in 2022.
For a cost measure to be scored, an individual MIPS eligible clinician or group must meet or exceed the case minimum for that cost measure.
One Cost Measure – If only one cost measure can be scored, that measure’s score will be used to compute a cost performance category score.
Multiple Cost Measures – If multiple cost measures are scored, the cost performance category score is the equally-weighted average points assigned to the scored measures. For example, if 7 out of 25 cost measures are scored, the cost performance category score is the equally weighted average of the 7 scored measures.
None – If none of the cost measures can be scored, the cost performance category will count toward 0% of your MIPS final score, and CMS will reweight your performance category scores as follows: quality to 55%; improvement activities to 15%; and Promoting Interoperability to 30%.
To calculate the cost performance category score in 2022, CMS will assign 1 to 10 achievement points to each scored measure based on the MIPS eligible clinician or group’s performance on the measure compared to the performance year benchmark. As a result, the achievement points assigned for each measure depends on which decile range you or your group’s performance on the measure is between.
An individual or group’s cost measure performance is expressed as a dollar amount. A measure score (expressed as up to10 points from a benchmark decile) is derived by comparing your performance on the measure to the performance of all individual MIPS eligible clinicians, groups, and virtual groups who were evaluated on the measure.
Reweighting the Cost Performance Category
In circumstances where CMS may not be able to reliably calculate a score for any of the cost measures within the cost performance category that adequately captures and reflects the performance of a MIPS eligible clinician, CMS won’t calculate a score for the cost performance category and will redistribute the category weight to other performance categories.
CMS will automatically reweight the cost performance category for individual MIPS eligible clinicians who are located in a CMSdesignated region or locale that has been affected by extreme and uncontrollable circumstances. If a MIPS eligible clinician is located in an affected area, they’ll:
- Assume the clinician doesn’t have sufficient cost measures applicable; and
- Assign a weight of 0% to the cost performance category in the final score even if we receive administrative claims data that would enable us to calculate cost measures for that clinician.
Clinicians, groups, and virtual groups can also request reweighting of the cost performance category (and other performance categories) by submitting an extreme and uncontrollable circumstance exception application.
If other performance categories are reweighted, the cost performance category will always be weighted at either 30% or 0%—CMS won’t redistribute weight to the cost performance category for the 2022 performance year, except in cases when the cost and the improvement activities performance categories are the only 2 categories scored. In this case, both categories will receive a weight of 50%
Additional Resources
This guide details how to participate in the cost performance category of the Merit-based Incentive Payment System (MIPS) in 2022.
A guide to help clinicians get started participating in the Cost performance category of the Merit-based Incentive Payment System (MIPS) during the 2022 performance period.
2022 MIPS Cost Measures Code List
Details the codes used in the specifications for each of the 23 episode-based cost measures, the revised Medicare Spending Per Beneficiary (MSPB) Clinician measure, and the revised Total Per Capita Cost (TPCC) measure that are in use for the Merit-based Incentive Payment System (MIPS) cost performance category in 2022.
2022 MIPS Summary of Cost Measures
This document provides a summary of cost measures in use for the MIPS Cost performance category in 2022, as well as measures under development.
2022 MIPS Cost Measures Information Forms
Details the measure methodology for the 23 episode-based cost measures, the revised Medicare Spending Per Beneficiary (MSPB) Clinician measure, and the revised Total Per Capita Cost (TPCC) measure that are in use for the Merit-based Incentive Payment System (MIPS) cost performance category in 2022.
