Overview
The Promoting Interoperability performance category emphasizes the electronic exchange of information using certified electronic health record technology (CEHRT) to improve:
- Patient access to their health information,
- The exchange of information between healthcare providers, and
- The systematic collection, analysis, and interpretation of healthcare data.
For 2022, the Promoting Interoperability performance category for traditional MIPS:
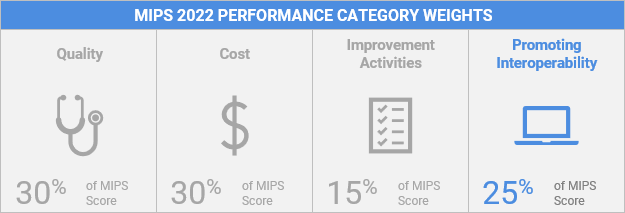
- Is worth 25% of your MIPS Final Score.
- Has a minimum performance period of 90 continuous days between January 1, 2022 and December 31, 2022.
- Uses performance-based scoring at the individual measure level.
- Requires 2015 Edition CEHRT, 2015 Edition Cures Update CEHRT, or a combination of both.
What’s New with Promoting Interoperability in 2022?
- Clinical social workers and small practices qualify for automatic reweighting of the Promoting Interoperability performance category beginning with performance year (PY) 2022.
- CMS added a new required, but unscored attestation measure, the High Priority Practices Guide of the Safety Assurance Factors for EHR Resilience (SAFER) Guides measure, beginning with PY 2022.
- CMS revised the Prevention of Information Blocking attestation statements to distinguish this attestation from the separate information blocking policies established in the 21st Century Cures Act final rule. This attestation has been renamed Actions to Limit or Restrict Interoperability.
- CMS revised the Public Health and Clinical Data Exchange objective requirements to support public health agencies during future threats and the long-term COVID-19 recovery process:
- Clinicians are required to report on the 1) Immunization Registry Reporting and 2) Electronic Case Reporting measures.
- CMS added a 4th exclusion for the Electronic Case Reporting measure, available for PY 2022 only.
- Clinicians are required to report on the 1) Immunization Registry Reporting and 2) Electronic Case Reporting measures.
- Clinicians can optionally report on the 1) Public Health Registry Reporting, OR 2) Clinical Data Registry Reporting, OR 3) Syndromic Surveillance Reporting measures for 5 bonus points.
Reporting/Submission Requirements
You must submit collected data for all required measures from each of the objectives (unless an applicable exclusion is claimed) for the same 90 continuous days (or more) during 2022.
In addition to submitting measures, you must provide your EHR’s CMS Certification ID from the Certified Health IT Product List (CHPL) and submit a “yes” via Attestation to:
- The Actions to Limit or Restrict the Compatibility or Interoperability of CEHRT (previously titled Prevention of Information Blocking) Attestation,
- The Security Risk Analysis measure, and
- NEW: The High Priority Practices Guide of the Safety Assurance Factors for EHR (SAFER Guides) measure.
When you report on required measures that have a numerator/denominator, you must submit at least 1 in the numerator if you do not claim an exclusion. Each measure is scored based on the MIPS eligible clinician’s performance for that measure (based on the submission of a numerator/denominator or a “yes or no” statement).
Objectives and Measures
The 2022 Promoting Interoperability performance category focuses on 4 objectives:
- e-Prescribing
- Health Information Exchange (HIE)
- Provider to Patient Exchange
- Public Health and Clinical Data Exchange
Within these objectives, there are 5 to 6 required measures (dependent upon which measure(s) you choose to report for the HIE objective) in addition to required attestations and optional measures.
| Objectives | Measures | Exclusions |
| ePrescribing | e-Prescribing | Any MIPS eligible clinician who writes fewer than 100 permissible prescriptions during the performance period. |
| ePrescribing | Bonus: Query of Prescription Drug Monitoring Program (PDMP) | Optional bonus measure (can report for 10 bonus points), no exclusion available. |
| Health Information Exchange | Support Electronic Referral Loops by Sending Health Information | Any MIPS eligible clinician who transfers a patient to another setting or refers a patient fewer than 100 times during the performance period. |
| Health Information Exchange | Support Electronic Referral Loops by Receiving and Reconciling Health Information | Any MIPS eligible clinician who receives transitions of care or referrals or has patient encounters in which the MIPS eligible clinician has never before encountered the patient fewer than 100 times. |
| Health Information Exchange | HIE Bi-Directional Exchange | Alternative measure, no exclusion available |
| Provider to Patient Exchange | Provide Patients Electronic Access to Their Health Information | No exclusion available |
| Public Health and Clinical Data Exchange | Immunization Registry Reporting (Required) | Refer to the measure specifications for detailed information on measure exclusions. |
| Public Health and Clinical Data Exchange | Electronic Case Reporting (Required) | Refer to the measure specifications for detailed information on measure exclusions. |
| Public Health and Clinical Data Exchange | Clinical Data Registry Reporting (Optional) | No exclusions available |
| Public Health and Clinical Data Exchange | Public Health Registry Reporting (Optional) | No exclusions available |
| Public Health and Clinical Data Exchange | Syndromic Surveillance Reporting (Optional) | No exclusions available |
Optional Query of Prescription Drug Monitoring Program (PDMP) Measure
The Query of PDMP measure continues to be optional for the 2022 performance period.
- You’ll receive 10 bonus points if you report a “yes” for the optional PDMP measure in addition to the required e-Prescribing measure.
- You can’t report the optional PDMP measure if:
- You claim an exclusion for the e-Prescribing measure.
- You don’t use CEHRT to electronically prescribe at least one Schedule II opioid.
Optional Public Health and Clinical Data Exchange Measures
To earn an additional 5 bonus points for the Promoting Interoperability performance category, clinicians can optionally report on one of the following measures:
- Public Health Registry Reporting
- Clinical Data Registry Reporting
- Syndromic Surveillance Reporting
Required Attestations
Security Risk Analysis Measure – The Security Risk Analysis measure is a required but unscored measure. This measure addresses the security (including encryption) of electronic personal health information (ePHI) data created or maintained by CEHRT, requiring, as needed, the implementation of security updates and correction of identified security deficiencies as part of the MIPS eligible clinician’s risk management process.
In addition to the required measures, you must conduct or review a security risk analysis on your 2015
Edition CEHRT and/or 2015 Edition Cures Update CEHRT functionality on an annual basis, within the
calendar year of the performance period. During the submission period, you will attest to the Security Risk Analysis measure by entering a “yes” (analysis completed) or “no” (analysis not completed) response.
High Priority Practices Guide of the SAFER Guides Attestation Measure – The High Priority Practices Guide of the SAFER Guides measure is a required but unscored measure.
There are 9 SAFER Guides which are organized into 3 groups: foundational guides, infrastructure guides, and clinical process guides. The High Priority Practices SAFER Guide is one of the foundational SAFER Guides. The guide helps healthcare organizations identify “high risk” and “high priority” recommended safety practices intended to optimize the safety and use of EHRs.
In addition to the required measures, you must conduct an annual self-assessment of the High Priority Practices SAFER Guide during the calendar year in which the performance period occurs. MIPS eligible clinicians are expected to fill out the checklist and practice worksheet at the beginning of the guide.
During the submission period, you will attest to the High Priority Practices SAFER Guide attestation measure by entering a “yes” (completed a review of the guide) or “no” (did not complete a review of the Guide) response.
Office of the National Coordinator for Health Information Technology (ONC) Direct Review Attestation – An ONC Direct Review is the process by which the ONC may directly review certified health information technology (IT) or a developer’s actions or practices to determine whether conform to the requirements of the ONC Health IT Certification Program. This attestation statement aims to identify whether you acted in good faith and would cooperate if the ONC initiates a direct review of your health IT.
During the submission period, you will complete the ONC Direct Review Attestation statement by entering a “yes” (agree to cooperate in a direct review of your health IT in the event that you receive a review request from the ONC) or “no” (you don’ not agree to cooperate in a direct review) response.
Actions to Limit or Restrict the Compatibility or Interoperability of CEHRT Attestation – To prevent actions that block the exchange of health information, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) requires eligible clinicians that participate in the Promoting Interoperability performance category to show that they have not knowingly and willfully limited or restricted the compatibility or interoperability of their CEHRT.
Eligible clinicians are required to show that they are meeting this requirement by attesting to the Actions to Limit or Restrict the Compatibility or Interoperability of CEHRT statement about how they implement and use CEHRT.
During the submission period, you will complete the Actions to Limit or Restrict Interoperability Attestation statement by entering a “yes” (certify that you didn’t knowingly or willfully take action to limit or restrict interoperability or compatibility of CEHRT) or “no” (certify that you did knowingly or willfully take action to limit or restrict interoperability or compatibility of CEHRT) response.
Scoring
The promoting interoperability performance category is worth 25% of your MIPS Final Score in 2022.
CMS will score each measure by multiplying the performance rate (calculated from the numerator and denominator you submit) by the available points for the measure. The Public Health and Clinical Data Exchange measures will be awarded full points if a “yes” is submitted for 2 registries or one “yes” and one exclusion.
You must report all required measures (submit a “yes”/report at least 1 patient in the numerator, as applicable, or claim an exclusion) or you will earn a zero for the Promoting Interoperability performance category.
If exclusions are claimed, the points for those measures will be reallocated to other measures.
Example: If a MIPS eligible clinician submits a numerator and denominator of 200/250 for the e-Prescribing measure (worth up to 10 points), the performance rate is 80%. This 80% would be multiplied by the 10 total points available for the ePrescribing measure to determine the
measure score. In this case, the ePrescribing measure score would be 8 points.
Hardship Exceptions
You may submit a MIPS Promoting Interoperability Performance Category Hardship Exception Application, citing one of the following reasons for review and approval:
- MIPS eligible clinician using decertified EHR technology
- Insufficient Internet connectivity
- Extreme and uncontrollable circumstances
- Lack of control over the availability of CEHRT
If your hardship exception is approved, the Promoting Interoperability performance category will receive a weight of 0% when calculating your final score and the 25% will be redistributed to another performance category (or categories) unless you submit data for this performance category.
Some clinicians will be automatically reweighted based on:
- Their special status (for example, hospital-based clinicians),
- Their clinician type (for example, a physical therapist, occupational therapist, or clinical psychologist, or clinical social worker), or;
- If they are a part of a small practice.
These clinicians will not need to submit a Promoting Interoperability hardship exception application.
If you’re reporting as a group or virtual group all MIPS eligible clinicians in the group or virtual group must qualify for reweighting for the group to be reweighted, unless the group or virtual group has a special status that qualifies them for automatic reweighting.
Additional Resources
2022 MIPS Promoting Interoperability User Guide
A guide to help clinicians participating in the Promoting Interoperability performance category of the Merit-based Incentive Payment System (MIPS) during the 2022 performance period.
2022 MIPS Data Validation Criteria
Lists the 2022 criteria used to audit and validate data submitted for the Merit-based Incentive Payment System (MIPS) performance categories.
2022 Promoting Interoperability Measure Specifications
Provides a detailed overview of the requirements for the 2022 Promoting Interoperability performance category objectives and measures.
2022 Promoting Interoperability Quick Start Guide
A guide to help clinicians get started participating in the Promoting Interoperability performance category of the Merit-based Incentive Payment System (MIPS) during the 2022 performance year.
2022 MIPS Promoting Interoperability Hardship Exception Application Guide
A guide to help clinicians participating in the Promoting Interoperability performance category of the Merit-based Incentive Payment System (MIPS) apply for a hardship exception during the 2022 performance period.
