Overview
The Quality performance category measures your performance on clinical practices and patient outcomes. Quality measures are tools that help CMS assess health care processes, outcomes, and patient experiences to ensure they align with CMS quality goals for health care.
For the 2022 Performance Year (PY), Providers can select from more than 200 available quality measures. Data needs to be collected and submitted for each quality measure for the entire 2022 calendar year.
To meet the Quality performance category requirements, a MIPS eligible provider, group, or virtual group can report:
- 6 quality measures (including at least one outcome measure or high priority measure in absence of an applicable outcome measure) for the 12-month performance period; OR
- A defined specialty measure set (if the measure set has fewer than 6 measures, all measures within that set need to be submitted); OR
- All quality measures included in the CMS Web Interface, a collection type available to registered groups or virtual groups with 25 or more eligible providers.
Reporting Requirements
General reporting requirements (for those not reporting through the CMS Web Interface):
- You’ll typically need to submit collected data for at least 6 measures (including 1 outcome measure or high-priority measure in the absence of an applicable outcome measure), or a complete specialty measure set.
- You’ll need to report performance data for at least 70% of the patients who qualify for each measure (data completeness).
- You can submit measures for different collection types (except CMS Web Interface measures) to fulfill the requirement to report a minimum of 6 quality measures.
Data Collection Requirements
You must collect quality measure data for the 12-month performance period starting January 1 – December 31, 2022. If you fail to meet data completeness requirements, you will receive zero (0) points for the measure, unless you are a small practice, in which case you will receive three (3) points.
The data completeness requirement is 70%, which means that you need to report performance or exclusion/exception data for at least 70% of patients or encounters that are eligible for the measure’s denominator.
There are 6 collection types for quality measures:
- Electronic Clinical Quality Measures (eCQMs)
- MIPS Clinical Quality Measures (CQMs)
- Qualified Clinical Data Registry (QCDR) Measures
- Medicare Part B claims measures
- CMS Web Interface measures
- The Consumer Assessment of Healthcare Providers and Systems (CAHPS) for MIPS survey.
Submission Methods
There are 4 submission methods you can use for reporting quality measures, depending on what submitter type you are. The submission types are:
- Medicare Part B claims
- Sign in and upload
- CMS Web Interface
- Direct submission via API
Scoring
CMS determines measure achievement points by comparing performance on a measure to a measure benchmark.
If a measure can be reliably scored against a benchmark, it means:
- A benchmark is available.
- Has at least 20 cases.
- Meets the data completeness requirement standard, which is generally 70%.
- CMS Web Interface measures are scored against the Medicare Shared Savings Program benchmarks.
Quality measures submitted for the 2021 performance period will receive between 0 and 10 measure achievement points.
Bonus Points
As finalized in the CY 2022 Physician Fee Schedule Final Rule, CMS is removing bonus points for end-to-end electronic reporting and reporting additional outcome/high priority measures. This will allow for a shift towards a more simplified scoring standard focused on measure achievement.
Six bonus points will still be added to the quality performance category score for clinicians in small practices who submit at least 1 measure, either individually or as a group or virtual group. This bonus isn’t added to clinicians or groups who are scored under facility-based scoring.
You may also earn up to 10 additional percentage points based on your improvement in the quality performance category from the previous year.
Additional Resources
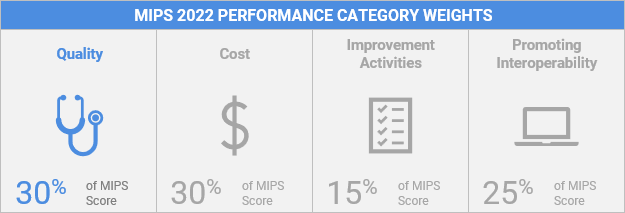
This guide details how to participate in the quality performance category of the Merit-based Incentive Payment System (MIPS) in 2022.
Lists and explains 2022 benchmarks used to assess performance in the quality performance category.
2022 MIPS Data Validation Criteria
Lists the 2022 criteria used to audit and validate data submitted for the Merit-based Incentive Payment System (MIPS) performance categories.
2022 Quality Quick Start Guide
A guide to help clinicians get started participating in the quality performance category of the Merit-based Incentive Payment System (MIPS) during the 2022 performance period.
